Using a Do Not Resuscitate order in real life
Interview with Ann Marie, Part 1
Welcome back to I’m Not Gaslighting You, the series about medical gaslighting and healthcare inequality, written from the perspective of a medical sociologist who also happens to be a real live woman in an actual body.
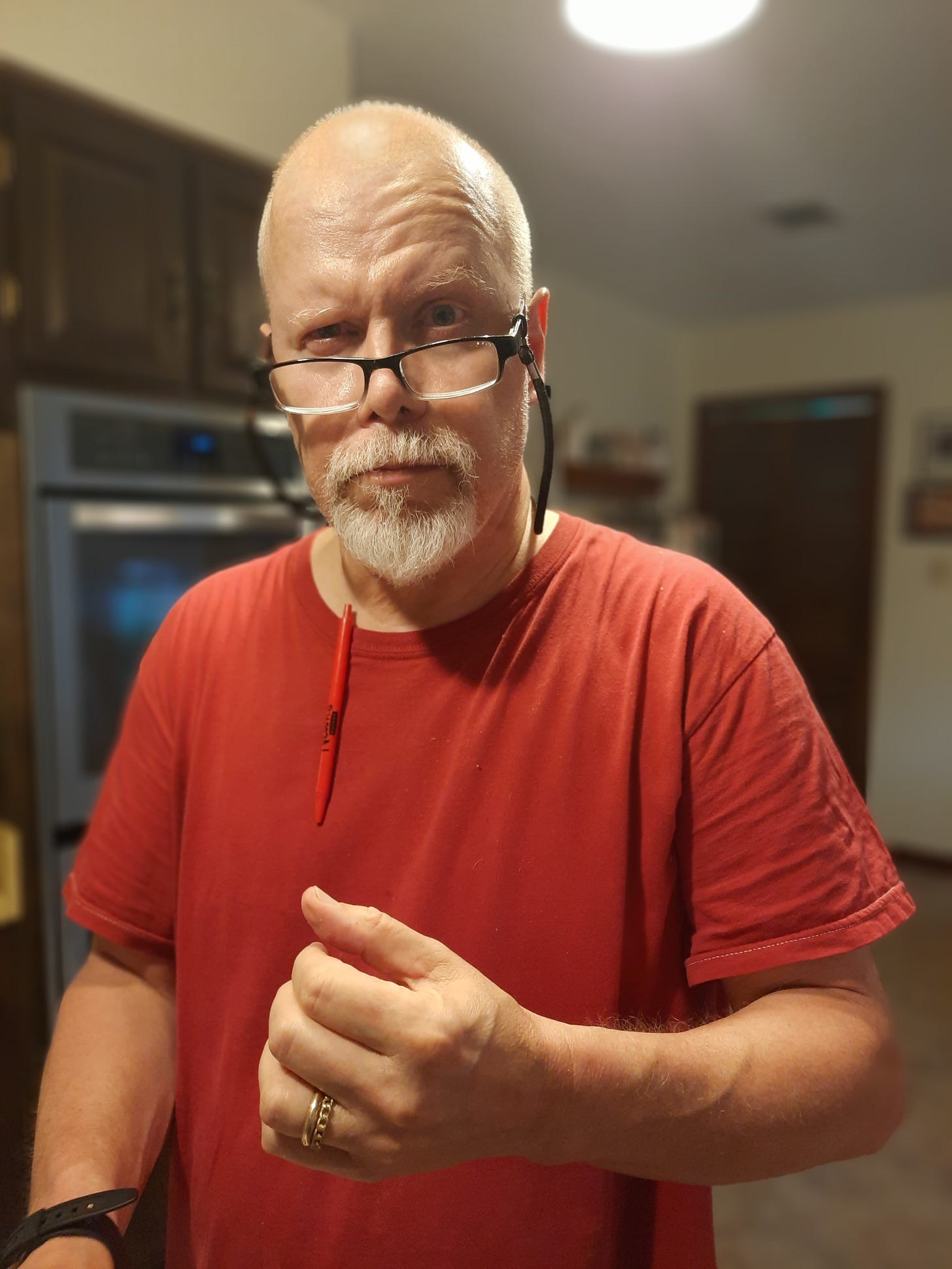
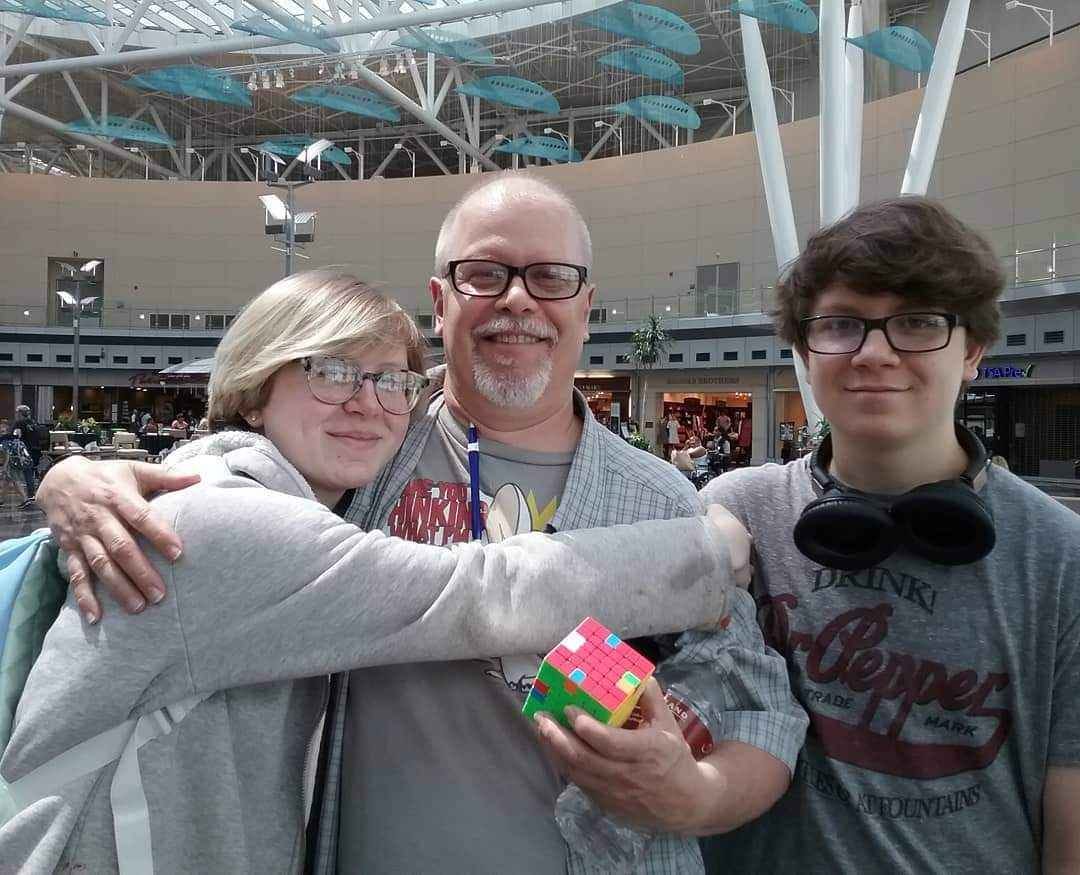
Today we’re doing an interview with my long-time friend and colleague, Ann Marie, about her experience with healthcare following her husband’s traumatic brain injury and death last year.
If you’ve ever wondered about how an advance directive plays out in real life, you’re going to want to hear Ann Marie’s story.
Ann Marie and I met back in 1993, when we were in graduate school together in Bloomington, Indiana. We shared an advisor and were both assigned to be teaching assistants for his class. Back then, grading exams meant that you actually had to haul around a big pile of hard copies, so you better be careful not to lose any of them or spill your coffee.
It also meant that you had to actually get together in person, which is to say I remember a bunch of Saturdays spent hanging out at Ann Marie and Kevin’s kitchen table in those early days. I have fond memories of them always being so welcoming to me. Ann Marie made me laugh this week when she reminded me how students used to try to route their papers to me because they thought she was the harder grader—they were shocked to find out we basically did it together!
Later, Ann Marie graduated, and they moved to Mississippi, having two lovely children along the way. Because her parents lived in Bloomington, sometimes Ann Marie would come home to visit and we could catch up. I remember one time we went to Dairy Queen in the hot summer when she was close to having her first baby. Most of the time since then, though, we’ve kept in touch through social media.
In early 2024, Ann Marie and her family went through something devastating, and as she posted about it online my old friend was on my mind, probably more than she knew.
One day at home, Kevin collapsed and hit his head, and was rendered unconscious. He had a traumatic brain injury, which landed him in the ICU for several weeks, still unconscious. From there, he moved to a specialty care hospital for another two weeks and then to a nursing home that had the capacity to take care of patients like Kevin who had tracheostomies.
During this time, Kevin never regained consciousness.
Ann Marie was holding down her job as a professor, their household, and parenting her children, who by then were 26 and 21 years old.
Thankfully, she and Kevin had conversations over the years about what they would want when it came to their end-of-life care. When Kevin was admitted to the nursing care unit, Ann Marie signed a Do Not Resuscitate (DNR) order. She was going back and forth to visit Kevin, trying to get him the best care and sustain the whole situation.
On Father’s Day 2024, Ann Marie visited Kevin, a bit later in the afternoon than her usual. When she walked into his room, she immediately noticed that he was not breathing normally. She sought a nurse and asked her to come look at Kevin, but the nurse did not seem overly worried as they had just finished a breathing treatment for him and he had seemed fine.
What followed was a rapid escalation. As soon as the nurse entered the room, she was alarmed and medical team rapidly assembled in the room. Ann Marie stood to the side, stunned and bewildered, trying to make sense of what was happening.
A major clue? The head floor nurse turned to Ann Marie and asked, “Do you want us to resuscitate him?”
This was of course confusing to Ann Marie since Kevin was breathing, albeit labored, so she was not anticipating the need for resuscitation. As she would learn later, Kevin’s heart had already stopped, which is why his breathing had changed but still continued.
Even more, she was thinking of that DNR order and mentally asking, “But didn’t I already decide this?? Do I have to answer again now??”
Perhaps mercifully, Kevin died before Ann Marie had to take this conversation further.

_____
When we caught up on the phone a few weeks ago, it was so good to hear Ann Marie’s voice. She had been reading my various social media posts and this column, and wanted to talk about her experience.
When she got to this point in telling me the story, she said she was also thinking to herself, “How am I supposed to tell you not to resuscitate the father of my children?” Even though she knew from years of talking with Kevin that he would not want to be kept alive in this condition, and she had signed the DNR, being asked this question in the moment was difficult and upsetting.
We decided to get together here to hash that out.
_____
Karen: Thanks for being here, Ann Marie. I’m so sorry for what you, the kids, and Kevin have been through. But I’m grateful you’re willing to talk about this, because I think other people would have the same questions as you: I filled out this advance directive, isn’t that sufficient to halt a resuscitation? How has your thinking about that moment evolved since that day?
Ann Marie: It really was a surreal experience. I knew something was wrong, more wrong than other times things had been “wrong,” but not “he’s-dying-right-this-minute” wrong. So when the nurse turned to me and said that, I was like, “Wait, what??” I am like, “Didn’t we already decide this when he was admitted? Why are we asking this now?”
And then I am thinking: If Kevin was answering the question, he probably would have never wanted to make it out of the ICU, given that he never regained consciousness and honestly was not doing well, so he would have definitely said “no” to resuscitation. But his children were still thinking/hoping he would recover (I was trying to stay optimistic with them, probably too optimistic) so in that way I felt “yes” to resuscitation.
So probably in 15 seconds all of these conflicting thoughts are going through my head. With the upshot being: “What kind of terrible person says no, don’t resuscitate?”
Honestly, again this sounds terrible, but I was actually relieved that Kevin made the decision for me by dying. It was less than a minute between being asked about resuscitation and then the announcement that his heart had stopped and he was gone.
Karen: I don’t think that sounds terrible at all— I think a lot of people are caught in such brutal decisions that they are relieved to have it taken out of their hands.
When we were on the phone, I asked if you were glad you were there in time for Kevin’s death, and I was really struck by your response. You said that you were glad to be there in time to be able to hold Kevin’s hand and tell him you loved him. But being there in time also meant you were disabused of the idea that death happens in a quiet, struggle-free way. Do you want to say more about that?
Ann Marie: I think, like many people, I had never been with a person as they were dying. Both my parents are still living. I thankfully have never lost a child. I lived across the country from my grandparents when they passed.
I guess since he had been in a coma state for months, I pictured the possibility of Kevin dying as just going to sleep and not waking up. The fact that your body can try to keep going even after your heart stops wasn’t something I had experience with.
He was so frail at that point, I am glad they hadn’t tried to pound his heart back into action. I think it would have broken him.
Karen: I love how you make this point. If we don’t have much experience with seeing people die, it’s hard to make these decisions in advance because it’s not clear what might happen.
You also made the point that now your children have had the experience of losing a parent, while your parents are still living. Do you have insights about how this might affect them differently, by virtue of being younger?
Ann Marie: Yes, my son pointed that out to me, that he and his sibling have an experience that I don’t since both my parents are still living. Although, in some ways losing Kevin was hard for them but it wasn’t totally unexpected.
One, Kevin was a fatalist who always thought he was going to die early and would tell the kids all the time that he hoped he lived long enough to see them graduate from high school (he did!). The fact that he made it to 65 was sort of a surprise to him. Two, he had been in a coma for months, and even though I was being as optimistic as I could with the kids, they knew things were not great.
But I do know that they are now very worried about losing me as well. Especially when five months after their dad dies, I get diagnosed with breast cancer.
They check on me a lot to make sure I am okay. I think now that I’ve been through chemo and radiation, and I seem to be doing well, they are a little less worried about being orphaned.
But I think they also wonder if when I tell them I am okay, I am being “optimistic” the way I was with Kevin. Which I understand.
I told them it was going to take time for Kevin to recover, but that he probably would. I didn’t do a great job of preparing them for the opposite, that he’s not going to recover. I guess because I didn’t really want to accept that he would not recover. But my parents do the same thing to me. Lol!
Karen: Such an important question— how to maintain optimism and hope while also preparing for the possibility that someone dies.
Ann Marie has great insights on this— so much that we divided this interview into 2 posts. Next time, we get her thoughts on do-overs in healthcare, how to think about advocating for your loved ones, and how conversations need to be combined with advance directives to be their most effective. Stay tuned!
End Notes:
Ann Marie, what are you reading?: Unruly: The Ridiculous History of England’s Kings and Queens I bought it in a bookshop in Kensington on my last study abroad trip. It’s quite humorous.
What are you watching?: I am a K-drama addict! It’s ridiculous how many K-dramas I’ve watched. I just finished Bon Appétit, Your Majesty. It was pretty good.
Do you have Substack recommendations? You are the only one I actually follow although I do like getting the Weekender and dipping into various posts as I have time or interest. I also subscribe to three newspapers, several other new sources like the AP, and education and nonprofit newsletters. Between all that and what my oldest child shares with me on Instagram, I am feeling a bit overwhelmed by all of it!




Hi Karen,
Thank you for sharing Ann Marie's story. It's so devastatingly and powerfully told.
I was completely struck by that one, awful moment. The nurse asks, "Do you want us to resuscitate him?" and Ann Marie's stunned thought is: "But didn’t I already decide this?? Do I have to answer again now??”
It’s this heartbreaking moment where the "official" document, the DNR, completely fails to protect her from the brutal, emotional reality of the moment. It's the gap between the protocol and the pain.
My novel, "What Was Here," is obsessed with that exact gap.
It's about a child in a Gaza camp who, to cope, builds his own bureaucracy—a 'Ministry' with logbooks, "protocols," and a "seal". He desperately wants his protocols to be real, to be stronger than the chaos. He logs a death as "Status: Pending. Location: Under review" or misspells a name "forever" because the seal has been applied.
Ann Marie's story is the devastating, real-world truth of what happens when those systems we build to protect us just... fail... in the face of life and death.
Since your post explores this so beautifully, I thought the story might resonate. You can read it here: https://silentwitnessin.substack.com/p/what-was-here?r=6r3orq
Thank you for this powerful interview.
This really resonated with me. I work in Home Health and I’ve been alone with a patient in their home when they went into cardiac arrest and because unresponsive. I called 911, the paramedics arrived within minutes and started to fly into action. That’s when I found his signed DNR on the fridge and yelled “Wait!” Everything stopped. We followed his wishes and he passed away. It was an emotional moment, but I’ve always been so grateful to him that he had his wishes so clearly posted. Thanks for writing about this. These conversations are so important.